 Image by braineater via Flickr
Image by braineater via Flickr
Wednesday, February 24, 2010
More Linky Love: Xyrem, Lyrica & Neurontin, Oh My!

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Sunday, February 21, 2010
Linky Love: What Are Other People Saying About Xyrem?
 Image by melanie_hughes via Flickr
Image by melanie_hughes via Flickr

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Saturday, February 20, 2010
My Friend Buys a Condo & Gets a Home Buyer Tax Credit
 Image by Rockin Robin via Flickr
Image by Rockin Robin via Flickr
- First-time home buyers and those who have not owned a home in the last 3 years are eligible
- Those eligible can receive up to an $8,000 federal tax credit
- Income limits are $125,000 for single persons and $225,000 for married couples
- To take advantage of the program, you must act by April 30, 2010
- There may not be another extension of this tax credit program
Click here for even more information: Home Buyer Tax Credit

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Thursday, February 18, 2010
Xyrem: How Does This Make Sense?
 Image by caseywest via Flickr
Image by caseywest via Flickr
- If you take Xyrem, you need to be in bed and ready to go to sleep, because within minutes of taking it, your body will be paralyzed.
- If you get out of bed, you risk falling and injuring yourself.
- You risk having an "accident" in bed (so maybe an adult diaper is in order.)
- I personally know someone who took this medication and did not fall asleep. Instead, she lay in bed paralyzed for 4 hours, unable to move, completely awake.
- You take this medication in two nightly doses, about 4 hours apart (i.e. it only lasts for 4 hours.)
- There are side effects like nausea, although the prevailing prescribing wisdom is to have the patient take a large enough dose that they just sleep through the side effects.

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Wednesday, February 17, 2010
A Pleasant Side-Effect
 Image by caseywest via Flickr
Image by caseywest via Flickr

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Tuesday, February 16, 2010
Out of Order
 Image by snacktime2007 via Flickr
Image by snacktime2007 via Flickr

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Wednesday, February 10, 2010
Patients for a Moment #16: Four Letter Words

Welcome to the 16th edition of the Patients for a Moment (PFAM) blog carnival. This is my first time hosting PFAM and I really enjoyed the experience. Thanks to Duncan Cross for allowing me to pose this Valentine's Day inspired question:
Love? Hate? What are the four letter words you use to describe your life with chronic illness?I enjoyed reading all the submissions and found a whole range of four letter words that describe life with chronic illness. They include: real, help, much more, near and dear, full, work, care, muse, loss, miss, risk and defy.
REAL
In a post that is a true expression of love, Ashley of Lymenaide: living in Harmony with Lyme submitted a post written by her husband Sander about her struggles with Lyme disease. Ashely educates us that in her husband's native Australia, the term fair dinkum means real. This post touched my heart as Sander describes the real sacrifices he has made to help Ashely get on the road to recovery from Lyme disease. Read Lyme is a Fair Dinkum Disease.
HELP
Trudy of A New Beginning: My Life with RSD starts by talking about love, then gets to the heart of the matter. After being diagnosed with Reflex Sympathetic Dystrophy in 2005, Trudy needed a whole lot of help from her husband with just about everything when she lost the use of her hands. Her post illustrates what can happen when a marriage transforms from a husband and wife team to a patient and nurse relationship. Read Keeping Love Alive During Illness.
MUCH MORE
"The word pain just sounds so insignificant," Jolene of Graceful Agony: Living your best life despite chronic pain states. For something that impacts her life so completely, she thinks pain should be a word that is bigger, bolder and commands more respect and attention. Her post reminds all of us who live with chronic pain that pain is what we feel, not who we are. In her post she invites us all to get to know much more about who Jolene really is despite living with chronic pain. Read Pain is a 4 letter word.
NEAR & DEAR
Annie's blog title is both provocative and full of truth: It's Time To Get Over How Fragile You Are. Tired of life being dictated by her health problems, Annie endeavors to be proactive about really living. Annie shares with us a "beautiful lie" from her childhood and her discovery that chronic illness has brought her more love from the people that are near and dear to her than she ever thought she would have in her life. Read Love and Chronic Illness.
FULL
Laurie at A Chronic Dose ponders the roles of love and hate in her 29 year journey with chronic illnesses. On the one hand, she notes that time and acceptance have helped her not feel hatred when she thinks of the various losses linked to her health struggles. On the other, she admires how she has figured out how to build a life full of things she wants to do and how she fortifies it against the attempts of illness to take little pieces away from her. She realizes that living a full life means she doesn't have to hate her illnesses. Read Give and Take.
WORK
Take a trip through time with Lisa at the blog Brass and Ivory, brought to you by the four letter word work. Her post demonstrates how chronic illness can change the course of a life through its up and downs. Her definition of work has changed over time and, yes, managing health problems is work. Yet despite it all, she shows us how our desire to work--to shape, form and improve ourselves and proceed towards goals or along a path--still remains. Read Illness in One Word: WORK.
CARE
Enjoy a little Valentine's Day whimsy with a poem written by Dot at Fibro World. Like she says, living with fibromyalgia might be blue, but the support of all the people she cares about helps her get through. Read Fibro Valentine: Roses Are Red, Fibro Is Blue...
MUSE
Sharon at After Gadget: Facing Life After the Loss of My Service Dog writes a loving and touching post about her life with her "hindrance dog." It seems that life with Gadget didn't start out very well, but after struggles and frustrations during training he transformed into a magnificent helper on which she came to rely. Though he is no longer with Sharon, the memories of their time together now bring her happiness and Gadget lives on as her blogging muse. Read Sick Humor Retro: The Hindrance Dog.
LOSS
Living with illness brings many changes to our lives, both visible and invisible. Kelly at Rheumatoid Arthritis Warrior took the time to create a list of 20 ways RA has changed what she sees when she looks in her mirror. Her simple list recounts for us of all the little ways illness creates loss in our lives. Read 20 Signs of Rheumatoid Arthritis in the Mirror.
MISS
All too often part of the illness experience is letting go of previous life plans and careers that just don't fit any more. Finding yourself on the path not taken can make you feel totally lost and missing your old, pre-illness life. Diana from Somebody Heal Me: the musing of a chronic migraineur shares with us what it feels like now that chronic migraines have taken away her ability to pursue her dream profession. Read Lost: Chronic Pain Erased My Plans.
RISK
How difficult it must be to know that each time you eat a new food you risk worsening your Crohn's disease and suffering some very unpleasant, gut-twisting consequences. Such is the life of Duncan from Duncan Cross: ill. humored who is the founder of the PFAM blog carnival. Food is his four letter word, and until science comes up with a better way for him to get nutrition, he is resigned to having to eat it. Read Food is a four-letter word.
DEFY
My contribution to this edition of the PFAM blog carnival is a post about the words can't, won't and don't, which symbolize the barriers and limitations people with chronic illness face. While it is true there are things I can not do or change, I can defy those limits by focusing on the can's, do's and will's that still exist in my life. I'm rediscovered my fighting spirit, striving to live my best life despite chronic illness. Read Can't, Won't, Don't.
That's all for this edition of Patients for a Moment. Join us next time when Leslie from Getting Closer to Myself hosts on February 24th. Her question for us then:
What’s Illness Got To Do With It? What is your relationship to illness? Is there a particular time when you wish illness wasn’t in the picture? Or is there a time when you find it’s easy to forget about illness?

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Tuesday, February 9, 2010
Can't, Won't, Don't
 Image by Henry0 via Flickr
Image by Henry0 via Flickr
I've been thinking about the four letter words associated with my life with chronic illness a lot lately in my role as host for the upcoming February 10th edition of the Patients for a Moment blog carnival. Words like cope, pain, fear, hate, ache, hard, rest, pace, heal, ouch, sigh, woes and hope. Yet for some reason the combination of can't, won't and don't kept rolling around in my head over the past few days...
Pronunciation: \ˈkant, ˈkänt, especially Southern ˈkānt\
: can not
Examples:
- The long-term disability insurance company says: We can't pay benefits for more than two years for someone with fibromyalgia and chronic fatigue syndrome.
- I say: I can't do as much as I used to do because pain and fatigue limit me.
Pronunciation: \ˈdōnt\
1 : do not
2 : does not
Examples:
- The doctor says: I don't think there is any reason for you to come back and see me again. I don't think there is anything more I can do for you.
- I say: I don't feel good. The doctors don't really know what is wrong with me and they don't really have anything to give me to make me better.
Pronunciation: \ˈwōnt; New England, upstate NY, nPa ˌwənt, ˈwənt; greater NYC ˈwünt; eSC ˈwünt, ˈwu̇nt\
: will not
Examples:
- My spouse says: You won't be able to keep going to those appointments because we can't afford the out-of-pocket costs.
- I say: I am having a bad day and I won't be able to meet up with you like we planned.
In my teens and 20's, words like can't, don't and won't were akin to waving a red cape in front of a bull. Anyone speaking those words, telling me what I wasn't able to do got a passionate 'F*** you!' as a response. I then proceeded to show that person they were absolutely wrong: I could, I would and I did.
In my 30's, I felt the bile rise in my throat when people I supervised as social work program manager uttered those words. I was all about getting things done for our clients and I tried very hard to inspire others to rise up and eliminate barriers by knocking them down or figuring out how to get around them. I came to view people who talked in can'ts, don'ts and won'ts as lacking motivation, creativity and determination.
Now in my 40's and living a life with chronic illness, I have to accept that there are some things I can not do or change. For the first few years of my transition into this new life, I got pretty upset when ever I ran into people who believe there wasn't anything wrong with me or focused on their limitations and inability to help me. That's when I came full circle. I somehow found my passion to once again prove the nay-sayers wrong by finding reasonable and appropriate things I could do despite my chronic pain and fatigue. I also started cutting loose those people focused on their limits and unable to think outside of the box for new and novel ways that could help me. I got it that chronic illness is really all about self-management of symptoms like pacing, resting, planning and saying no and self-help approaches to coping like play, pray and support from others.
So go ahead, chronic illnesses, keep telling me I can't, won't and don't. This tired and achy babe still has a fire in her belly and is ready to take you on. I've got more life to live and I'll be damned if I am going to let you take it away from me. I'm on a mission to live my best life despite chronic illness and that mean focusing on can, do, does and will.
~definitions courtesy of Merriam-Webster.com
This post is sponsored by Medi-Gap Policies.com. Find the best Medicare supplemental insurance rates in your area: medicare supplement plans

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Walking in My Shoes
 Image by moriza via Flickr
Image by moriza via Flickr

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Monday, February 8, 2010
What is the Autonomic Nervous System?

I'm looking at the image I added to this blog post and nodding my head. This may be one of those posts that don't require many words. So maybe I'll just highlight the main concepts and let the images and the table below do most of the talking today.
The autonomic nervous system works 24/7/365, i.e all the time. Humans have very little control over what autonomic nervous system does, with the exception of breathing. Some individuals can be trained with biofeedback techniques to influence, but not control, heart rate and blood pressure.
The autonomic nervous system has three components: the sympathetic nervous system, the parasympathetic nervous system and the lesser known enteric nervous system. The sympathetic nervous system controls the "flight or fight" response in our bodies, the "Oh no, there is a lion! Let's get out of here!" response. The parasympathetic nervous system controls the "rest and digest" response. The enteric nervous system is known as our second brain and is located in our gut, although why we need a second brain surrounding our stomachs is still unknown.
Here is a summary of how the sympathetic and parasympathetic nervous systems effect some of our internal structures and organs (chart courtesy of the Neuroscience for Kids website):
| The Autonomic Nervous System | ||
| Structure | Sympathetic Stimulation | Parasympathetic Stimulation |
|---|---|---|
| Iris (eye muscle) | Pupil dilation | Pupil constriction |
| Salivary Glands | Saliva production reduced | Saliva production increased |
| Oral/Nasal Mucosa | Mucus production reduced | Mucus production increased |
| Heart | Heart rate and force increased | Heart rate and force decreased |
| Lung | Bronchial muscle relaxed | Bronchial muscle contracted |
| Stomach | Peristalsis reduced | Gastric juice secreted; motility increased |
| Small Intestine | Motility reduced | Digestion increased |
| Large Intestine | Motility reduced | Secretions and motility increased |
| Liver | Increased conversion of glycogen to glucose |  |
| Kidney | Decreased urine secretion | Increased urine secretion |
| Adrenal medulla | Norepinephrine and epinephrine secreted |  |
| Bladder | Wall relaxed Sphincter closed | Wall contracted Sphincter relaxed |
In dysautonomia, the sympathetic and parasympathetic responses become dysregulated. One way to measure the responsiveness of the autonomic nervous system is through a test called a heart rate variability study. You may be surprised to learn that a normal heart does not beat at regularly timed intervals. Apparently looking at a heart beat pattern reveals the state of the autonomic nervous system.
According to the results of my heart beat variability study done back in 2005, my heart does beat in a more regular pattern, which indicates that both my sympathetic and parasympathetic systems have less tone or responsiveness. It also showed that overall my sympathetic nervous system was more active than my parasympathetic nervous system. This explains why the my symptoms of dysautonomia trouble me so much, because my body spends way more time in "fight or flight" than "rest and digest."
If a picture is worth a thousand words, you will now begin to see how disconcerting and uncomfortable it might be to live in a body where all your automatic functions are revved up and out of sync.

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Sunday, February 7, 2010
PFAM 2/10: Love, Hate and Other Four Letter Words
 Image by doryexmachina via Flickr
Image by doryexmachina via Flickr
This is the last call for submission for the February 10th edition of the Patients for a Moment (PFAM). Per the PFAM guidelines, the deadline to submit your published blog post to the host (that would be me!) is by the end of the day today. I am looking forward to reading the submissions and admiring the creativity that abounds in the blogging community.
I wonder how many four letter words I am going to find in the blog posts submitted. I'm excited to hear the your answers to the following query.
Ah, February! Valentine's Day will soon be here and love is in the air. Or is it, if you are a patient for a moment? Is love still in your vocabulary or has it been replaced by other four letter words? Let us all know when you submit your blog post answering this question:
Love? Hate? What are the four letter words you use to describe your life with chronic illness?
I am accepting submissions until 11:59 PM PST today, so there is still time to join PFAM by contacting me.

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Friday, February 5, 2010
How Do You Get Dysautonomia?
 Image by Bob.Fornal via Flickr
Image by Bob.Fornal via Flickr
Today I want to talk a bit about how you get dysautonomia. Let's start with a tidbit from the National Dysautonomia Research Foundation:
Autonomic dysfunction can occur as a secondary condition of another disease process, like diabetes, or as a primary disorder where the autonomic nervous system is the only system impacted. These conditions are often misdiagnosed.I believe that I have been living with dysautonomia for at least 12 years, but it wasn't until 2007 that I was "officially" diagnosed with the disorder. Several doctors misdiagnosed me with panic or anxiety disorders before the true cause of my symptoms was identified (see my post from yesterday to get my take on this issue.)
Here is a list of factors that can lead to the development of dysautonomia, adapted from the dysautonomia article at Wikipedia:
- Genetic factors - often results in the most severe cases of dysautonomia
- Hereditary connective tissue diseases (i.e. Ehlers-Danlos Syndrome)
- Exposure to chemicals (i.e. chemotherapy for cancer treatment)
- Viral illness (Hepatitis C?)
- Compression of important arteries and/or nerves (Thoracic Outlet Syndrome?)
- Pregnancy
- Diabetes and other autoimmune disorders
- Parkinson's disease and other degenerative neurological diseases
- Physical trauma or injury which damages the autonomic nervous system
- Brain injury
While my cancer treatment history is probably the primary reason I have dysautonomia, I have highlighted some of the other medical conditions I have that appear on this list. Seems I have three additional medical conditions that are risk factors for developing dysautonomia. I wonder how my chronic Hepatitis C infection, Thoracic Outlet Syndrome and Type 2 diabetes affect my dysautonomia. At the very least, being vigilant about keeping my blood sugar under tight control seems important to prevent my dysautonomia from getting worse. This is also one of the reasons I want to treat my Hepatitis C infection when antiviral drugs become available. As for Thoracic Outlet Syndrome, there doesn't seem to be much I can do about it: surgery to attempt to correct the problem isn't an option for me.
I also want to mention here that there is a prominent doctor and researcher from Mexico City, Dr. Manuel Martínez Lavín, who believes that dysautonomia is at the root of fibromyalgia. You can read more about his theory here. I believe that Dr. Martínez Lavín is on to something and I am the perfect case study to prove his theory.
To end these series of posts on dysautonomia, my next blog entry will attempt to explain what the autonomic nervous system is and does. Stay tuned!

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Thursday, February 4, 2010
Dysautonomia: A Clarification
 Image via Wikipedia
Image via Wikipedia
I really don't want you to get the wrong idea about dysautonomia, so today I need to take a step back and clarify a key point.

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Wednesday, February 3, 2010
OMA&P! Hosting the PFAM Blog Carnival 2/10/10
 Image by laurenmarek via Flickr
Image by laurenmarek via Flickr
Love? Hate? What are the four letter words you use to describe your life with chronic illness?

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
When Things Just Don't Work Right
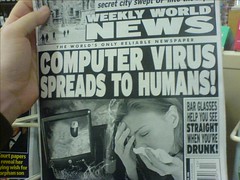 Image by TedRheingold via Flickr
Image by TedRheingold via Flickr
I've been battling spy ware and malware on my computer all yesterday, trying to get rid of the viruses and restore my computer to good health. In biology there is a word for that: homeostasis. That is when all the parts of the human body work together to achieve a stable, functional state. Just like my computer, if you introduce a virus, the human stable state is disrupted. Our bodies strive to return us back to homeostasis, a process we know better as healing.
After a visit yesterday with my neurologist, I acknowledge once again that my body has not returned to normal yet either. I really like my neurologist because she listens to me and understands how complicated things are inside my body. Yesterday we talked a lot about my dysautonomia and how it prevents me from returning to homeostasis. I told my doctor that I understand she can not fix me. I just want her to figure out ways to help me manage my symptoms better and restore some function. She agreed that this was reasonable, but would take some out-of-the-box thinking.
Unlike my computer which will get fixed one way or another, we can't just reboot my autonomic nervous system. I walk a very thin line between feeling not good and feeling not crappy. Literally, my nerves are so sensitive that a stressful thought, a swing in my blood sugar, too much traffic on the street, too much loud noise from the neighbors or too much fatigue makes my body just start shouting. My body overreacts and my heart starts racing, my palms start sweating and my body feels shaky and faint.
As we discussed at my appointment, once my body starts shouting, no amount of meditation, visualization, guided imagery, focused breathing or positive thinking can make it stop. It's like being on a roller coaster, realizing as you pull away from the platform that you have changed your mind and want to get off and being overcome with terror as you start climbing the first incline with no escape in sight. White knuckling it, you are stuck on that roller coaster until it pulls back into the station. I constantly remind myself that I need to just breath and just wait it out. Because so far, whether it's a few minutes or a few hours, the symptoms do dissipate eventually.
My only consolation is that I have two wonderful doctors who really listen and are willing and able to help me through these episodes. They are my neurologist and my cardiologist. I hit a real low in 2007 when my dysautonomia was so bad I felt really agitated and thought I was going to have to been heavily sedated. Just out of the hospital, I was absolutely prostrated and yet I felt the need to pace the floor because I had so much nervous energy. Thank goodness I found these doctors since then and I will not have to go through that alone again. Which is a good thing because I think my Christmas present (aka menopause) is making my dysautonomia worse.
I left my appointment today hopeful that my neurologist will be struck by inspiration and new, novel treatment ideas will be born. I anticipate things we haven't tried yet and insights we hadn't considered. We both want me to achieve homeostasis again. We both feel less than happy about my current state of functioning. I like that she can empathize with my situation and not feel discouraged or defeated by it. I am rooting for her, with her education and experience, to figuratively pull a rabbit out of her hat. Maybe she will surprise me and do just that...
As for my computer, well I haven't given up on it either. I will figure out a way to get it back into an operational state. It is amazing how disruptive losing your homeostasis can be, whether you are a computer or a human being.

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
Monday, February 1, 2010
Can You Hear My Heart Beat, Heart Beat?
 Image by Stephen Poff via Flickr
Image by Stephen Poff via Flickr
- dysautonomia
- chronic fatigue
- chronic pain
Dysautonomia is a general term used to describe a breakdown, or failure of the autonomic nervous system. The autonomic nervous system controls much of your involuntary functions. Symptoms are wide ranging and can include problems with the regulation of heart rate, blood pressure, body temperature and perspiration. Other symptoms include fatigue, lightheadedness, feeling faint or passing out (syncope), weakness and cognitive impairment.

Like this post? Then please...

Submit it to your favorite social sites.
Share it with PrintFriendly alternatives.
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=7640ece9-f07c-46e7-80a1-3cb041e8bf98)

![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=0a546773-bee5-46c0-8315-6a4e057cf66b)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=2a6151bf-a497-4c4b-95bb-93c6e4158a21)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=f5738c51-d107-4de8-a63e-681dc1a810b7)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=a408e7e3-1b3c-46a5-bf4d-eb78e1e9898f)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=e3d5b732-988e-42bd-bcf8-a9b3a2f7b260)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=5198022f-9ecb-4ff5-b8e4-f11d688ecab8)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=02d8ea89-d5c9-45b4-a9f5-767cf01a2d52)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=939989a0-4870-4f89-9807-f901b28b5062)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=7b26320b-6ba8-4f3b-a669-f9080d9b79e7)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=5ddd6501-87ab-4601-b394-afdcf93d182f)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=d41d0013-934e-4002-858f-12ec6949bcf8)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=d0ace1a0-fa5b-48e3-915e-7dd2fecc9857)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_b.png?x-id=b63c7d54-5597-460e-8a20-8404040c41e5)